Direct Anterior Hip Arthroplasty
Dr. Rodriguez-Elizalde performs all hip replacements using the Direct Anterior Approach (DAA) using state-of-the-art surgical navigation (IntelliJoint Surgical Navigation System). The direct anterior approach has gained significant popularity in the U.S. and Canada as the preferred method of hip replacement. Dr. Rodriguez-Elizalde has performed thousands of successful DAA total hips over the last 10 years, and was the first to perform the procedure in the Greater Toronto Area.
The direct anterior approach involves operating from the front of the thigh to reach the hip joint. In traditional hip replacement, surgeons use the side (lateral) or back (posterior) approach, which involves cutting and reattaching of the tendons and muscles to reach the hip.
In the direct anterior approach, access to the hip is achieved between the muscles, eliminating the need to cut major tendons and muscles. This allows the patient to have more stability post-operatively and less immediate surgical pain. This translates to a faster recovery compared to traditional hip replacement.
Keep in mind that most hip replacements typically function at a similar level 6 to 12 months after surgery. The direct anterior approach to hip replacement has proven beneficial during the immediate post-operative period, with long-term outcomes on par with other methods.
Dr. Rodriguez-Elizalde is currently using the HANA Table, which was specially designed to aid in the direct anterior approach by Dr. Joel Matta. Dr. Matta is credited with bringing the DA technique to North America from France more than 30 years ago. The HANA Table controls the leg, allowing for rotation and elevation of the femur (thigh bone) during surgery, making the DAA possible.
It is important to remember that the direct anterior approach to hip replacement is still major hip surgery. There is associated surgical pain and swelling, so recovery varies from patient to patient. In our experience, the direct anterior approach has allowed for a faster rehabilitation on average, but setbacks and complications can still happen – as with any surgery.
Download Dr. Rodriguez-Elizalde’s Pre-Habilitation Program
No amount of online information can replace a visit with an orthopedic surgeon to determine if you would benefit from a hip replacement. This serves as a guide only. Hip replacement is an option in patients who have evidence of hip arthritis and have:
- Hip pain that significantly limits walking or other everyday activities. Hip arthritis is only one of the many causes of pain around the hip. (Other causes of hip pain include back issues, tendon, muscle or other soft tissue problems.)
- Tried non-surgical options that have not adequately helped with their pain/function
- Good underlying health. Patients who have had recent cardiac events, heavy smokers, poorly controlled diabetes, morbid obesity, or dementia, are at high risk for complications after hip replacement surgery
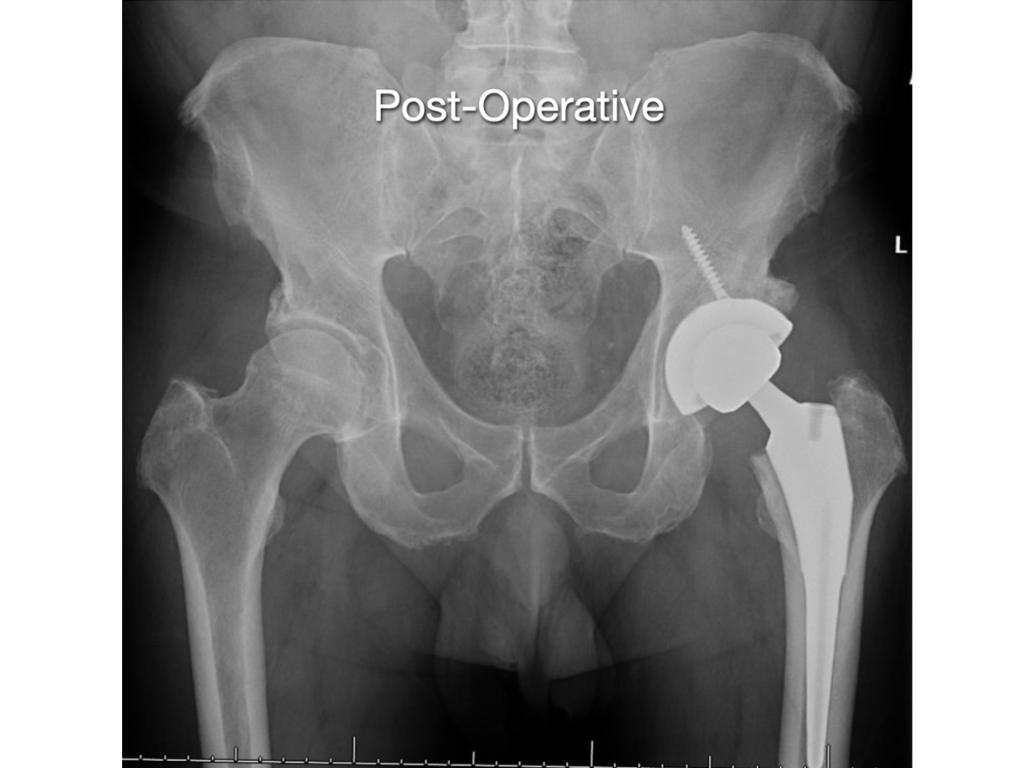
Hip replacement surgery replaces the femoral head with an artificial ball. The ball is “potted” into the thigh bone with a metal stem. A metal shell and plastic liner is inserted into the acetabulum (socket). This acts to replace both the ball and socket of the hip and helps alleviate the pain from hip arthritis
The anterior approach to hip replacement is gaining popularity because the recovery for patients is faster during the first 12 weeks after surgery, compared to other approaches. The “approach” means the direction a surgeon can take to get to the area of interest. Hip replacement can be “approached” from the back (posterior), side (lateral) or front (anterior). The anterior approach is a muscle-sparing approach that goes between muscle groups, rather than through them or having to detach major tendons.
It is important to note that there is no difference between the approaches in terms of the implants used or the long-term outcome of hip replacement. No approach is pain-free, so patients do need to expect surgical discomfort after any hip replacement. This discomfort dissipates significantly over the first 2 weeks post operatively.
Most of our patients after Anterior Hip Replacement are able to walk with a walker and do stairs within a few hours of surgery. Because the immediate surgical pain after the Anterior Approach is so much less compared to other approaches, most of our patients after Anterior Hip Replacement are able to go home the same day of surgery.
We use a special operating table called the “HANA Table” for Anterior Hip Replacements. It allows us to move your leg easily and to check our work using low-dose x-ray during the procedure, if necessary.
Rarely, patients are not candidates for the anterior approach (patients with ankylosing spondylitis, skin infection near the incision site, and some revision surgery)
Dr. Rodriguez-Elizalde performs nearly all hip replacements as day surgery procedures. The day of your surgery, you will mobilize with a physiotherapist using a walker, and be shown how to navigate stairs safely. After surgery, you can put your full weight on your operated leg, and have no post-operative restrictions.
Once comfortable, you will be discharged home with a prescription for painkillers, blood thinners and anti-inflammatories. You will see Dr. Rodriguez-Elizalde 7-10 days after surgery in the fracture clinic where your would will be examined, and your progress checked.
The next visit is at 5-6 weeks and involves a clinical check and x-rays. Overall, in terms of recovery, you will likely need a walker or cane for the first 2-4 weeks. A rough estimate of a timeline is a 60% improvement at 6 weeks, and an 80% improvement at 12 weeks. The most common complaints are stiffness, ache and swelling in front of the leg. Your deep “arthritic joint” pain should be gone the minute you wake up from surgery.
It is important to keep in mind that recovery varies for everyone. Dr. Rodriguez-Elizalde prefers to monitor your progression versus going by an absolute timeline. As long as you continue to improve week to week, you are doing well.
The answers to this varies quite a bit, depending on what you do, what accommodations can be made for you at work and at home, your expectations, your determination, and the amount of progress you make. Most “desk” type jobs can be resumed after about one month. Most physical jobs will need a longer recovery, typically 3-4 months.
An important factor in your return to work is your pre-operative fitness level. This cannot be stressed enough. The more your prepare, exercise, and become more fit, the easier your overall recovery will be.
You may drive when:
- You are no longer taking narcotic pain medication.
- You have full power and function to engage in emergency braking of your car if necessary.
This usually takes 4-6 weeks, but in some cases, patients if they meet the above criteria, can resume driving in as little as 2 weeks if they meet the above criteria.
After your hip replacement has healed, you may return to all day-to-day activities. In terms of recreational activities, patients may return to skating, skiing, weight lifting, swimming, bowling, golfing, tennis, biking and using an elliptical trainer. The only restriction is high impact jumping and running type activities. This is more Dr. Rodriguez-Elizalde’s personal preference, as there is no direct medical evidence that those activities cause early failure. That being said, running and jump cause very high joint reactive forces through the hip, and thus are thought to lead to earlier implant failure.
Ideally, flying and long distance travel can be resumed six weeks after surgery. Short flights and travel can be undertaken after 2-7 days after surgery, if necessary, but you should get up and move every hour, and will require a prescribed blood thinner.
Your largest consideration for travel should be how you feel. Keep in mind, you may still need a walker or cane to mobilize safely, and will be moving through crowded areas. Planes, buses and trains are cramped and sitting for long periods of time will cause stiffness and pain in the hip.
In summary, if you can delay your travel for the first 6 weeks, you will certainly enjoy your trip more. Short flights, and those necessary for returning home after surgery should not be considered before 2-7 days after surgery and will require a prescribed blood thinner.
No. This is different than Dr. Rodriguez-Elizalde’s previous recommendations where a dose of antibiotics was to be given prior to any dental procedures for life. In reviewing the recent literature and position of the American Dental Association, the use of antibiotics prior to dental work is not necessary.
We ask you to wait 3 months since after your surgery before going to the dentist.
There is no association of hip and knee infection with or without administration of antibiotics before dental work – so we have changed our policy and no longer require you take them.
Most patients experience a patch of skin numbness, about the size of their hand just beyond the incision site of an anterior hip replacement. This patch of skin numbness will not affect your function.
Often after hip replacement, the operated leg may be slightly longer than before surgery. This is often favourable because arthritic hips are often shorter than non-arthritic hips. Dr. Rodriguez-Elizalde will use either x-ray or computer navigation technology during your hip replacement surgery in an attempt to make lengths as even as possible during surgery. A leg length difference of more than 1 cm after surgery is very rare, unless there was a leg length difference before surgery. Many leg length differences immediately after surgery “even out” with time as the pelvis adjusts.
Some blood loss during hip replacement is normal. Blood loss requiring a blood transfusion after surgery is extremely rare unless you are anemic (low hemoglobin levels) before surgery, or you are having both your hips replaced at once. You will be sent for blood work when you book your surgery to make sure that you are not anemic. If you are anemic before surgery, we will refer you to our Patient Blood Management Coordinator who may suggest ways to build up your hemoglobin levels prior to your surgery.
The lifetime risk of a serious infection after a hip replacement is approximately 1%. Some of these infections occur soon after surgery, but most occur months or years afterwards. The treatment for serious (deep) infections includes revision surgery and IV antibiotics.
More commonly, patients can get less serious infections “cellulitis”, which can often be treated with antibiotics that can be taken by mouth. Sometimes surgeons will opt to “wash out” a skin infection in the operating room if the cellulitis gets serious.
People at higher risk for infection includes patients with poorly controlled diabetes, patients with morbid obesity (BMI more than 40), patients who are immunocompromised, or are taking immunosuppressant drugs, patients with peripheral vascular disease and smokers. An ongoing infection at the time of surgery from another source (eg, active urinary tract infection, tooth abscess, diabetic foot infection) can increase your risk of infection after surgery.
In order to prevent infection, your surgeon will give you one dose of antibiotics through your IV in the operating room before your surgery. You will get another dose after your surgery.
The symptoms of infection include fevers, redness around the wound, persistent leaking from the wound and increasing pain in a previously well-functioning joint replacement. If you think you are developing an infection around your hip replacement, call your orthopedic surgeon’s office as soon as possible or go to your nearest emergency department.
Blood clots in leg veins can occur after hip surgery. Dr. Rodriguez-Elizalde will prescribe a medication for you to take after your surgery in order to prevent blood clots. If a clot develops in a deep leg vein (deep vein thrombosis – DVT) above the knee, it will need to be treated with stronger blood thinners. Above knee DVTs need to be taken seriously because they can cause clots that go to the lungs (pulmonary embolus), which is a serious condition. If you have previously had a DVT, please let your surgeon know prior to your surgery.
It is normal to have some soreness in the hip after anterior hip replacement. This soreness typically improves significantly over the first six weeks after surgery. Some people still experience soreness up to 3-6 months after surgery. Barring complications, hip replacement surgery can hip with 85-90% of hip pain at the three-month mark. It is important to know that although most patients enjoy improved function, improved mobility and significant pain relief after recovery, a hip replacement may not feel like a “normal” hip.
Although unusual, hip dislocation is when the ball of the hip replacement comes out of the socket. This historically was a major complication, mostly associated with surgical approaches to the hip.
The anterior approach to the hip is the safest approach to minimize risk of dislocation – but the risk still exists.
If this happens, you will know that something is wrong and will need to go to your nearest emergency department to have the hip put back into place. The most common reason this happens is bending forward or twisting awkwardly. Other reasons for hip dislocation include infection, component malposition and shortening of the leg after surgery. The risk of dislocation is highest in the first three months after surgery. Recurrent hip dislocations sometimes require revision surgery. The risk of hip dislocation after the anterior approach is theoretically lower than the risk of dislocation after the posterior approach.
The metal components of the hip replacement are meant to bind with your bone in the first 3-6 months after surgery. Over the years however, this bond can loosen, requiring a revision of the components. Less common causes of early loosening include infection or failure of the components to bond to bone after implantation.
Damage to major blood vessels or nerves causing permanent muscle weakness is exceptionally rare, especially from the anterior approach.
Sebastian is an Orthopedic Trauma and Adult Hip and Knee surgeon at Humber Hospital, in Toronto, with a special interest in revision and complex cases.
He completed his orthopedic surgery residency at the University of Ottawa, after which he was accepted for Fellowship training at the Hospital for Special Surgery in New York, in Hip and Knee Arthroplasty.