Direct Anterior Hip Arthroplasty
Dr. Rodriguez-Elizalde currently performing all his hip replacements via the Direct Anterior approach (DAA). The DA has gained significant popularity in the US, and some centers in Canada as a preferred method of hip replacement.
The DA technique involves operating from the front of the thigh to reach the hip joint. Traditionally, surgeons used the side (lateral) or back (posterior) approach, which involves the cutting and reattaching of the tendons and muscles to reach the hip.
Anteriorly, access to the hip is achieved between muscles, eliminating the need to cut major tendons and muscles. This allows the patient to have more stability post-operatively and less immediate surgical pain. This translates to a faster recovery compared to traditional hip replacement.
Things to remember are that at 6-12 months, most hip replacements are functioning at a comparable level. The DA technique has been shown to aide in the immediate post-operative phase, but the long-term results are likely equivalent.
Dr. Rodriguez-Elizalde is currently using the Hana Table, which was specially designed to aid in the DA technique by Dr. Joel Matta. Dr. Matta is credited with bringing the DA technique to North America from France over 20 years ago. The Hana table controls the leg, allowing for rotation and elevation of the femur (thigh bone) during surgery, making the DA possible.
It is important to remember that DA Hip Replacement is still major hip surgery. There is associated pain, swelling and recovery varies from patient to patient. In our experience, the DA technique has allowed for a faster rehabilitation on average, but setbacks and complications can still happen – as with any surgery.
- FAQ
- Risks of Direct anterior Hip Arthroplasty
What is my expected recovery?
Almost all hip replacements done by Dr. Rodriguez-Elizalde are performed as day surgery. The day of your surgery, you will mobilize with a physiotherapist using a walker, and be shown how to navigate stairs safely. You can put your full weight on your operated leg, and have no post-operative restrictions.
Once comfortable, you will be discharged home with a prescription for painkillers, blood thinners and anti-Inflammatories. You will see Dr. Rodriguez-Elizalde 7-10 days after surgery in the fracture clinic for examine the wound and to check your progress.
The next visit is at 5-6 weeks, and involves a clinical check and x-rays. Overall, in terms of recovery, you will likely need a walker or cane for the first 2-4 weeks. A rough estimate of a timeline is a 60% improvement at 6 weeks, and 80% at 12 weeks. The most common complaints are stiffness, ache and swelling in the front of the leg. Your deep “arthritic joint” pain should be gone the minute you wake up from surgery.
The most important thing to remember is that recovery varies for everyone. Dr. Rodriguez-Elizalde prefers to monitor your progression vs an absolute timeline. As long as you continue to improve week to week, you are doing well.
Back to work?
This question varies a lot on what you do, and any accommodations that can be made for you at work and at home. Most importantly is depends on you – your expectations, drive and recovery are all variable. Most “desk” type jobs can be resumed around 1 month later, sooner in some cases. Most physical jobs will need a longer recovery, typically 3-4 months.
Ultimately, recovery depends on your pre-operative fitness level
This cannot be stressed enough.
The more you prepare, exercise and are fit, the easier overall recovery is.
Driving?
You may drive when:
1) You are no longer taking narcotic pain medication
2) You have full power and function to engage in emergency braking
of your car if necessary.
This usually takes 4-6 weeks, but in some cases, patients if they meet the above criteria, can resume driving in as little as 2 weeks.
What activities can I do?
After your hip replacement has healed, you may return to all day-to day activities. In terms of recreational activities, patients may return to skating, skiing, weight lifting, swimming, bowling, golfing, tennis, squash, biking and use of an elliptical trainer. The only restriction is high impact jumping and running type activities. This is more Dr. Rodriguez-Elizalde’s personal preference, as there is no direct medical evidence that those activities cause early failure. That being said, running and jumping cause very high joint reactive forces through the hip, and thus are thought to lead to earlier implant failure.
Flying/Travel
Flying and long distance travel should ideally only be done 6 weeks after surgery. Short flights and travel can be undertaken after 2-7 days after surgery if necessary, but you should get up and move every hour, and will require a prescribed blood thinner.
The largest hindrance of travel is how you are feeling. You may still need a walker or cane to mobilize safely, and will be moving through crowded areas. Planes, buses and trains are cramped and sitting for long periods of time will cause stiffness and pain in the hip.
In summary, if you are able to delay your travel for the first 6 weeks, you will certainly enjoy your trip more. Short flights, and those necessary for returning home after surgery should not be done before 2-7 days, and will require a prescribed blood thinner.
The HANA Table
The HANA® table is a specially designed surgical table that allows for hyperextension, adduction and external rotation of the hip to an extent not possible with conventional tables. This allows Dr. Rodriguez-Elizalde to perform Direct Anterior Approach Total Hip Arthroplasty safely and effectively.
Developed by California-based Mizuho OSI, the table’s name – Hana® – is an acronym that stands for Hip And kNee Arthroplasty surgical table. http://www.mizuhosi.com/products/orthopedic-fracture-trauma/hana/
In 1996 Dr. Joel Matta, who had observed anterior hip replacement in Paris, rethought his approach to hip replacement. By abandoning the posterior approach and adopting the anterior approach his goals were: lower chance of dislocation, enhanced recovery rate, and increased accuracy of hip prosthesis placement and leg length.
Dr. Matta is now recognized as the originating orthopaedic surgeon performing Direct Anterior Hip Arthroplasty in North America. He also is the co-designer of the new and improved anterior hip replacement operating room table. The current iteration of this table is the Mizuho OSI Hana table, and is in use at Humber Hospital by Dr. Rodriguez-Elizalde.
Do I need Antibiotics Before a Dental Procedure?
No. This is different than Dr. Rodriguez-Elizalde’s previous recommendations where a dose of antibiotics was given prior to any dental procedure for life.
In reviewing the recent literature and position of the American Dental Association, the use of antibiotics prior to dental work is not necessary. http://www.ada.org/en/member-center/oral-health-topics/antibiotic-prophylaxis
There is no association of hip or knee infection with or without administration of antibiotics before dental work – so we have changed our policy and no longer require you take them.
1) Infection
Occurs in approximately 1% of primary (first time) surgical cases, and 5-10% or revisions (re-do surgery). Superficial skin infections can usually be treated by oral antibiotics, but may necessitate the use of IV antibiotics as well. Careful sterile technique and the use of antibiotics during surgery have greatly minimized the risk of infection over the years.
If a deep infection occurs, surgery may be necessary to clean out the hip joint, and possibly replace the prosthesis with a temporary spacer. This spacer is made out of cement loaded with high dose antibiotics which leach into the surrounding tissue to combat the infection. This is reinforced with a regime of IV antibiotics for several weeks. Once the infection is cured, a definitive replacement can be performed.
2) Peri-Prosthetic Fracture
A Peri-Prosthetic fracture (break around the hip implant) at the time of surgery or soon there after occurs 0.5% of the time. This is usually age related, with a higher incidence in those with osteoporosis. Excessive stiffness or deformity may also increase the risk of fracture.
The treatment varies on the timing, location and severity of the fracture. Simple cracks might just involve altering the weight-bearing status of the patient for 4-6 weeks after surgery. Other fractures may involve surgery – either to fix the fracture, or exchange any loose components.
3) Dislocation
Occurs in approximately 1% of primary (first time) surgical cases, and 8% or revisions (re-do surgery),with most dislocations occurring within the first six weeks of surgery. Traditionally, hip replacement patients needed "Hip Precautions" or limitations after their surgery. Repeated or traumatic dislocations may require further surgery to definitively stabilize the hip.
If you have undergone a Direct Anterior Hip Replacement, there are no precautions following surgery. You may gradually increase your activity level and range of motion.
However, Dr. Rodriguez-Elizalde performs most of his revisions through the posterior approach which requires "Hip Precautions" post surgery for the first 6 weeks. These are usually lifted at your 6 week follow up visit, after examination by your surgeon.
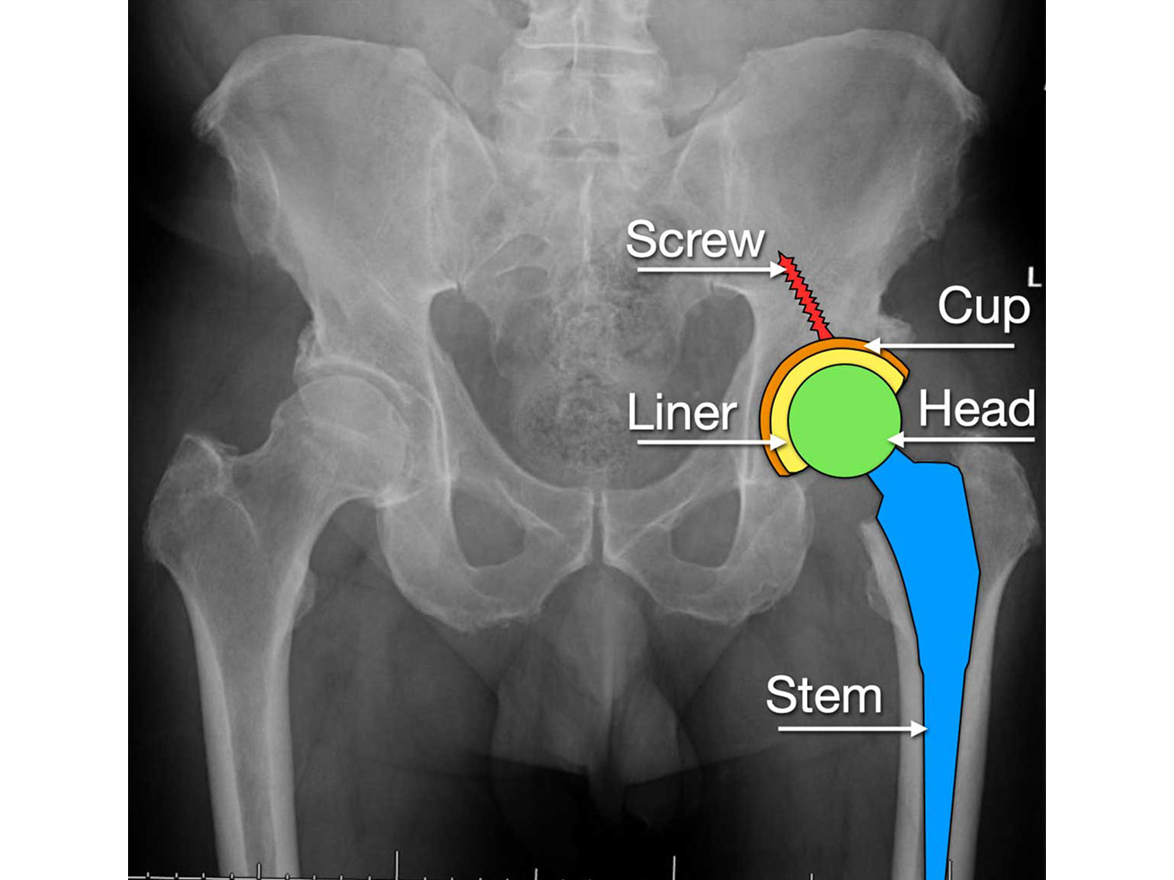
4) Revision
Hip revision surgery (re-do surgery) can happen due to infection and dislocation as outlined above, but also for loosening. Over time, hip replacements will wear eventually may change position due to loosening. Newer implants and articular surfaces are designed to last longer, but are still subject to wear.
Revision surgery is more involved that primary (first time) hip replacement surgery. Sometimes only one of the components (implants) needs to be removed or replaced. Often, the entire previous construct needs to be removed and replaced. The results of revision surgery vary depending on the reason for the revision. Overall, the outcome is good, though not as predictable as primary hip surgery.
5) Numbness
The lateral femoral cutaneous nerve crosses the surgical site in the Direct Anterior Approach. It is affected approximately 30% of the time, causing a temporary “palsy”, or numbness.
This resolves slowly with time, and may cause tingling or burning on the outside of the thigh. In 5% of cases, patients may be left with some permanent numbness on the outside of their thigh – this is just skin numbness and has no long-term impact on function or strength.
6) Major Nerve or Blood vessel damage
Nerve damage can occur in 0.1% of cases, most commonly in complex revision surgery. Major nerve damage can result is a “Drop Foot” or partial paralysis and numbness of the lower extremity. The recovery is slow, and often incomplete. Skin numbness from the surgical incision is a direct result of cutting the skin, and considered normal. This slowly recovers with time.
Blood vessel damage, like nerve damage is very rare, but can have serious consequences. An urgent vascular repair and/or transfusion of blood products may be necessary.